Fighting the Battle with Mud Fever
Author: Cedric Chan, MRCVS of NW Equine Referrals, familiarises us with equine pastern dermatitis, better known as ‘mud fever’. Here he tells us about the recent study he has conducted using the Equi-Med Ag products and reveals some interesting findings.

Fighting the Battle with Mud Fever
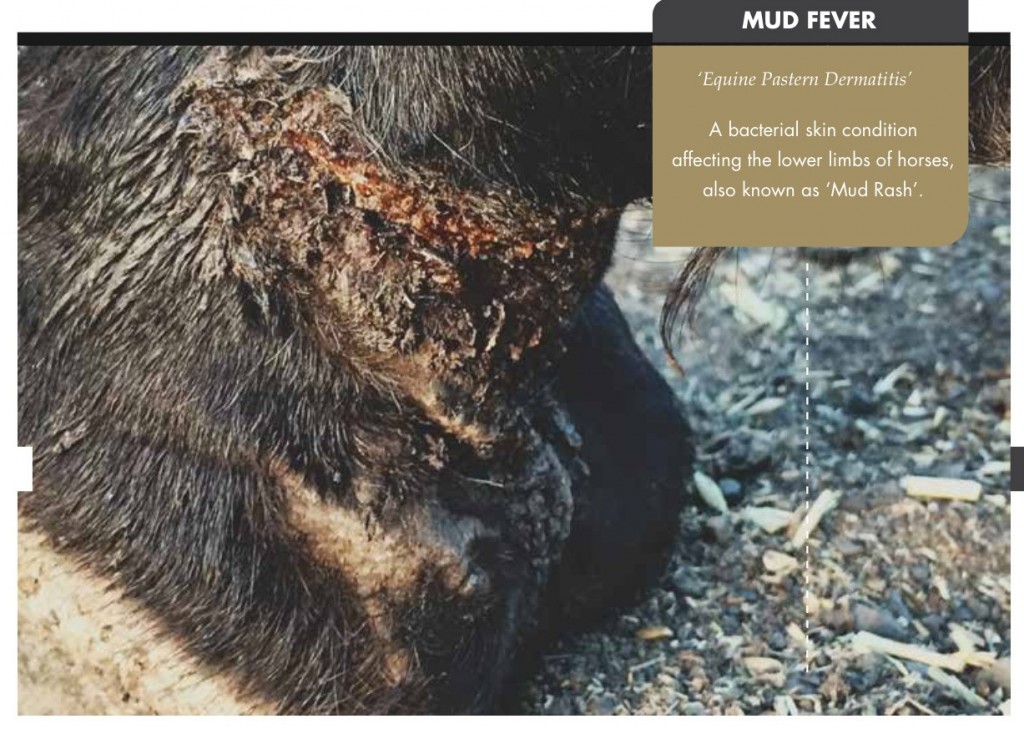
Mud fever is a colloquial term for a bacterial skin condition affecting the lower limbs of horses and has a variety of presentations (also known as mud rash, cracked heels, greasy heel, scratches, dew poisoning or grapes depending on the severity of the condition).
The scientific veterinary term used for all these conditions is ‘equine pastern dermatitis’. It is a very common condition that affects the pastern, fetlock and cannon region of horses, ponies and donkeys all over the world.
The bacterium Dermatophilus congolensis is often associated with the condition but we are now finding other bacteria are also present including Staphylococcus spp. and Pseudomonas aeruginosa. However, these are often not the primary cause but are secondary skin infections and reoccurrence is common.
Causes…
If an underlying cause of the condition can be understood and accurately diagnosed before treatment of any mud fever case, this would minimise the frustration of going through several failed treatments.
Although it can affect any breed of horse, it is most commonly associated with horses that have a lot of feather around their heels (Cobs and Draught types). Other predisposing factors can include poor stable/pasture conditions, moisture, sand, alkaline soil, poor fitting boots leading to trauma and poor grooming.
The condition usually affects the back of the heel and pastern but can spread around the side and the front, as well as over the fetlock and lower cannon. Hind limbs are more commonly affected than the front, and usually both hind limbs will become infected. It also seems to affect more adult horses than youngsters and occurs equally across the sexes. Also, it is often seen to affect horses with non-pigmented skin, but not exclusively.
There are also several primary factors that can directly cause mud fever including direct physical or chemical irritants such as blistering, treated bedding, immune contact allergy, vasculitis, ultra-violet sensitivity, fungal and parasitic infection.
Wet, muddy paddocks and sandy soil certainly worsen the condition, if not contribute to mud fever in the first place.
The signs…
Presentation of equine pastern dermatitis can vary depending on the cause, duration and any previous treatments.
It usually starts with generalised swelling of the affected area, redness and inflammation and scaling of the skin. This then progresses on to moistness, matting of the hair and scabbing or ‘crusting’.
As the skin immune defences lower a secondary bacterial infection is likely, often from the horse itself and/or the environment in the pasture or stable. The skin can become chronically thickened and split due to constant movement and the degeneration of a local healthy skin environment. As you can imagine it becomes very painful with varying degrees of lameness.
The study…
As mud fever was starting to become extremely difficult to treat and resolve with conventional treatments, I teamed up with a company, Equi-Med Ag Ltd., who had started to trial their products on horses using a new method of treatment and nothing else. Their results were so encouraging we sent the products, a wound dressing which contained activated carbon and nano-silver particles, to Lincoln University to be tested on the bacterium Dermatophilus and Psendomonas aeruginosa, which were known to cause mud fever.
The results showed that activated carbon in the Equi-Med Ag products retained and killed 99.9% of the bacteria it was tested on. It contains a unique combination of activated micro-porous carbon and nano-sliver particles which, it is claimed, is extremely effective in drawing out bacteria from the affected skin due to a constant electrostatic charge generated in the fabric surface. Once retained within the carbon structure, the bacteria engulf the nano-sliver particles and subsequently die outside the skin.
Two years after launching the products the team decided to do a more in-depth trial using actual cases with pastern dermatitis which took place during the summer months. After a nationwide appeal for severe longstanding cases, 30 applicants were chosen randomly from around the UK to take part. All cases had the condition at least six months or was a chronic recurrent condition.
Many of the cases had already tried standard veterinary treatments such as antibiotics, anti-inflammatories such as non-steroidal anti-inflammatory drugs and steroids, silver Flamazine and antibiotic-steroid cream, all of which had failed. Other cases had used adjunctive treatments such as Hibi-scrub, Manuka honey, shop bought creams and powders, all with no effect.
All the applicants followed the same study protocol for use of the EquiMed Ag wound dressing and preliminary bacterial swabs were taken and sent to Glasgow Veterinary School for analysis. The subjects then had the affected areas bandaged using the Equi-Med Ag wound dressing and were changed every three days.
It was important that the studies were carried out in the horse’s natural setting and not removed to a hospital centre to carry out the study to ensure the products worked effectively in a range of different settings in which they would be bought for. There was no change to the horse’s everyday management including turnout.
The results came back and showed that the bacterium Staphylococcus aureus was present in 90% of cases along with Psoudomonas spp and Streptococcus spp. However, interestingly from this initial study the bacterium Dermatophilus congolensis which was originally thought to have been the main cause of mud fever, was not present in any of the cases swabbed.
Each of the horses taking part in the study were all cleared within 2-6 weeks of treatment and all of them had no further signs of bacterial skin infections.
Changing how we think…

The Equi-Med Ag way may represent a new and ground-breaking approach to treating one of the most common and frustrating skin conditions known in the horse, by removing the need for traditional veterinary treatments, the high costs involved in unsuccessful and/or treating reoccurring cases, as well as reducing the need for long term broad spectrum antibiotic usage.
The absence of Dermatophilus congolensis isolated in this study suggests it is not the most common bacteria present in chronic cases of mud fever. However, its role in the initial stages of some cases has not been validated yet.
General advice with regard to prevention and on-going management of affected horses include a dry, clean environment, especially in wet weather. If stabled, keep on fresh, clean, untreated bedding that is regularly skipped out. If turning out, try to keep horses on drier pasture once the morning dew has subsided.
Horses with quite a lot of feather are best clipped over the pastern area to reduce the moisture retention. If ultra-violet light sensitivity is a factor then stabling and daily bandaging may be required.
The use of an antibacterial activated carbon and nano-silver dressing or impregnated boot, such as those manufactured by Equi-Med Ag Ltd. should be considered especially in severe and longstanding cases of mud fever.
Even horses who become very sensitive to touch and those with chronic swelling benefit from the boots and the dressing whilst making management of the condition and stable management routines much easier.
Case Study:
 Horse’s name: George
Horse’s name: George
Breed: TB x Arab mare
Age: 17
Colour: Chestnut
Rider’s name: Katie Lee
When I took George on loan I knew she had suffered in the past from mud fever through the winter months, and had previously had veterinary treatment which had failed to clear up the infection. I had tried every cream and topical treatment available but nothing seemed to really work that well.
After seeing an advert to take part in the Equi-Med Ag study I thought I would give it a try. We were now into the summer months and George’s condition had worsened and her legs were extremely sore and swollen.
Prior to using the Equi-Med Ag Wound Dressing her legs had become so sore and swollen that she hated me washing and touching her legs.
I soon realised ‘mud fever’ was a very generic term for pastern dermatitis and that it still could be a threat in the summer months. Through the study we discovered from the swabs that the strain of bacteria present was Staphylococcus aureus.
So I ditched the creams and topical treatments and treated her legs with the wound dressing, changing the dressing every three days. It was so simple to use, there was no need to keep washing her legs as I had done when I was using the creams.
Straight away after the first dressing change I could see the scabs had started to dry out, they looked darker and the redness and swelling in the affected legs had started to go. As I kept using the dressing the scabs started to fall away and I could see the skin and hair started to look healthy again.
After 27 days the scabs were completely gone and you couldn’t even tell where they had been.
The Equi-Med Ag products are so easy to use, cost effective and they really did work eliminating the bacterial infection in my case.
For more information on the Equi-Med Ag products visit www.EquiMedAg.com.au (Australia) or UK / Europe www.equimedag.co.uk